Leaked WPATH Recording: Navigating the 'Gender Journey' With 'Complex and Nuanced' Patients (Print Version)
A leaked recording of a session from the World Professional Association for Transgender Health's recent conference sheds light on how care providers approach complex cases of gender dysphoric adults.
Known for its lack of transparency, the World Professional Association for Transgender Health does not open its annual conference to reporters. Consequently, public accounts of what transpires within the confab can only come second-hand. However, a source leaked to me a recording of one of the WPATH conference sessions from its late-September gathering in Lisbon: “Understanding the Nuances Within the Rainbow: Navigating Challenging and Complex Clinical Cases.”
You can access the full audio of the session here:
Leaked Audio of WPATH Conference Session: “Understanding the Nuances Within the Rainbow"
Known for its lack of transparency, the World Professional Association for Transgender Health does not open its annual conference to reporters. Consequently, public accounts of what transpires within the confab can only come second-hand. However, a source leaked to me a recording of one of the WPATH
Below is a summary of this session, which exemplifies the delicate dance gender-medicine doctors choreograph as they seek to serve the wants and needs of trans patients while remaining cognizant of countervailing factors, such as severe psychiatric conditions or potentially contraindicating health problems.
The conference session was comprised of a virtual panel discussion by a multidisciplinary team from the Center for Gender Health at Hartford Health, which is Connecticut’s largest health care provider. The team zeroed in on three case studies of adults with gender dysphoria who presented with particularly complex care needs that prompted challenging clinical judgment calls.
Derek Fenwick, a psychologist and the clinic’s assistant director, served as panel’s moderator. He said that 20% of the clinic’s patient population “are more complex and nuanced” and thus “require some more consultation.”
The overriding theme throughout the session was that these providers are strictly opposed to treating gender dysphoria with any hint of the traditional paternalism for which doctors have long been notorious. “Shared decision-making,” as the model is known, was paramount as this team sought to work in partnership with these patients on what the panelists repeatedly referred to as their “gender journey.”
These three particular patients’ gender journeys, however, collided with various psychological and medical obstacles that at least appeared give these providers pause. Notably, never did the conference-session panelists make explicit that they might have weighed the risks versus benefits and ultimately refused to prescribe a treatment that the patient sought out—even if transitioning did not appear to be in the patient’s overall best interest, there was a medical contraindication, or the patient’s treatment expectations were unrealistic.
The apparent philosophy these providers followed is what Canadian transfeminine jurist Florence Ashley refers to as the effort to satisfy trans patients’ “embodiment goals.” The University of Alberta assistant professor of law has advocated for the dispensing of psychosocial assessments for people of any age seeking gender-transition treatment. She has asserted that all transgender care should follow an informed-consent model.
Accordingly, the Hartford Health providers made clear, as psychiatrist Dr. Carla Schnitzlein said, that they would never want to be “perceived as gatekeepers” by their patients.
Dr. Fenwick noted that new patients undergo a biopsychosocial assessment “that gives us a better understanding of the patient’s gender journey, which can then inform ways to help achieve their goals.” He repeatedly said that the team’s most important quest was to “meet the patient where they’re at.”
Steve or Jackie: a Potential Case of DID?
The first case considered a 47-year-old natal male who identified as bi-gender—as both a man and a woman. This patient alternated between two names and sets of pronouns: Steve (he/him) and Jackie (she/her). Because of this confusion and the fact that the patient often switched back and forth between these identities and the associated pronouns without warning, the care team referred to the person with they/them pronouns and as SJ or S & J.
SJ had been married for 20 years to a woman who remained in the dark about her husband’s gender identity. The couple had two “significantly disabled” teenage sons.
“I’m really never comfortable in my own skin,” SJ said, according to Laura Saunders, a psychologist and the center’s director. “I have dysmorphia and anxiety.” On multiple occasions, they bitterly said they were the “red-headed stepchild of the rainbow.”
It was quite evident that the care team did not care for SJ’s personality, which was irritable, abrasive and combustible.
After Dr. Saunders met with SJ, she referred him to Dr. Kelly Hamann, an endocrinologist on the team. Dr. Hamann said that SJ “presented very male to me in this initial intake.” But she immediately qualified this by saying, “And obviously, that’s a judgement on my part.”
Dr. Hamann said SJ was “almost beyond irritable” and “confrontational” and that they “started off basically telling me that [the care team wasn’t] going to meet their needs.” Like all her colleagues in the conference session, she emphasized working with patients to achieve their goals, or “our goals,” as she put it. She further said that part of her job was to screen for any health risks of gender-transition treatments.
“Anytime I’m saying that I think somebody needs a little bit more behavioral health screening, we in our discipline as psychiatrist, psychologist, therapist, could be perceived as gatekeepers, which is not something we want to do.”
The conundrum with caring for SJ was that the patient wanted breast development from estrogen treatment and possibly breast implants, but had still not told their wife about their bi-gender identity. Additionally, the care team puzzled over whether SJ might have dissociative identity disorder as the providers struggled to ensure that both of SJ’s identities—Steve and Jackie—would be consenting to any treatment.
According to Dr. Saunders, SJ’s outside therapist “really felt like the gender identity was rooted more in past trauma.” She continued: “It appeared to them to be a more of identity or dissociative split, not a true dissociative identity disorder. And in fact, they said that when they’ve tried to talk about this directly with SJ, they became very irritable and agitated, and so then became scared to talk about these issues with them.”
Dr. Hamann referred to potential use of estrogen for SJ as “gender-affirming hormone therapy,” which left unsaid the question of how using medication to affirm one gender might impact the other. She ultimately put the prospect of such treatment “on pause.”
Dr. Schnitzlein was eager to counterbalance such reluctance to prescribe hormone therapy with an assurance that the team was not there to tell people “no” or to make patients’ quest to obtain cross-sex hormones more cumbersome. “Anytime I’m saying that I think somebody needs a little bit more behavioral health screening, we in our discipline as psychiatrist, psychologist, therapist, could be perceived as gatekeepers, which is not something we want to do,” she said. What was important, she emphasized, was providing patients support “throughout the gender journey.”
Nevertheless, Dr. Schnitzlein said she looks for “diagnostic clarification and whether or not a psychiatric diagnosis impacts [a patient’s] ability or interferes with their ability to give true consent.”
The care team was also evidently reluctant to attribute a patient’s trans identity to past trauma. The suggestion that there is a cause-and-effect relationship between trauma and gender dysphoria remains highly controversial across gender medicine.
SJ made and canceled multiple appointments with a plastic surgeon to inquire about breast implants, which Dr. Saunders said spoke to the patient’s ambivalence. “How do you help navigate someone where maybe their goals don’t line up in a way that you’re expecting?” she said.
Such ambivalence notwithstanding, Dr. Hamann again stressed that she works in partnership with patients, even when their expectations or demands are unconventional. “I always tell them, I'm your wingman here. I’m here to help you get to where you want to be. I’m not here to tell you where you need to arrive,” she said.
Ultimately, SJ stopped returning to the clinic. So the care team was never compelled to make a judgment call about providing SJ with estrogen and breast implants. The conference panelists did not say what sort of treatment they might have advised had SJ remained a patient at the clinic.
Dan: Non-Binary With Type-1 Diabetes
The next case study concerned Dan, a 27-year-old natal male who identified as nonbinary and trans feminine and used he and they pronouns. Dan had type-1 diabetes, so he was already a seasoned endocrinology patient when he arrived at the clinic. Dan had gynecomastia, which is breast tissue build-up in men. But instead of wanting to lean into such a change in his body, Dan actually did not want any breast buildup. But he did want hormonal treatment that could provide him other feminine physical changes.
This presented Dr. Hamann with a challenge that she seemed eager to tackle in her effort to fulfill Dan’s desires. She discussed the possibility of using selective estrogen receptor modifiers, or SERMs, which are used for women with breast cancer. But she didn’t have much in the way of solid research go guide her prescribing. “There are some papers that look at the use of SERMs…in the trans population to achieve” feminization without breast development, she said. “But we don’t have any really significant, randomized controlled studies or long-term data about the effect of SERMs in the trans population.”
Dan, Dr. Hamann said, was still weighing his options. This has left her wanting more such options to meet the array of requests that trans and gender-nonconforming patients make. “I think that we do not have the entire spectrum of tools that we need to meet goals in gender-affirming health care,” she said. “I think that every year that marches on, we recognize more and more tools that we can use. For example, the use of GnRH agonists [used to block puberty in minors or suppress sex hormones in those past puberty] that are typically used for other purposes, now being used in our gender-nonconforming patients.”
Dr. Fenwick said that it was important to try not “to fit the patient into a binary box.”
“Even though there’s not a lot of studies out there” to guide the treatment, Dr. Fenwick said, it was important to try “to find other ways to get the desired goal for this patient, which is really important.”
“I’d rather acknowledge that sometimes I have egg on my face than lose somebody to life-saving care.”
Dr. Schnitzlein added that antidepressants could serve as a “floaty effect” to sustain patients’ overall mental health until they achieved the gender-transition treatment that would directly mitigate their gender dysphoria. However, she also that it was important to manage patients’ expectations of how such treatment might ultimately benefit them.
The panelists emphasized how important it was to gain the trust of a patient population that often has a history of, as they put it, health care trauma and is distrustful of doctors. This fraught dynamic presented an imperative to remain humble, said Dr. Schnitzlein. “If we do misstep” with patients, she said, “I’d rather acknowledge that sometimes I have egg on my face than lose somebody to life-saving care.”
Gary: a Trans Man With a Benign Tumor
The third and final case study concerned Gary, a 22 year-old natal female who identified as a trans male and had a history of severe psychiatric problems, including multiple hospitalizations and the repercussions of sexual trauma. At the time he presented to the clinic, he was also participating in an intensive outpatient program to “treat depression, anxiety, trauma and chronic suicidal ideation,” according to Dr. Fenwick.
It was remarkable to see how differently Dr. Hamann characterized Gary’s personality compared with SJ. She glowingly referred to Gary as a “lovely trans man individual.”
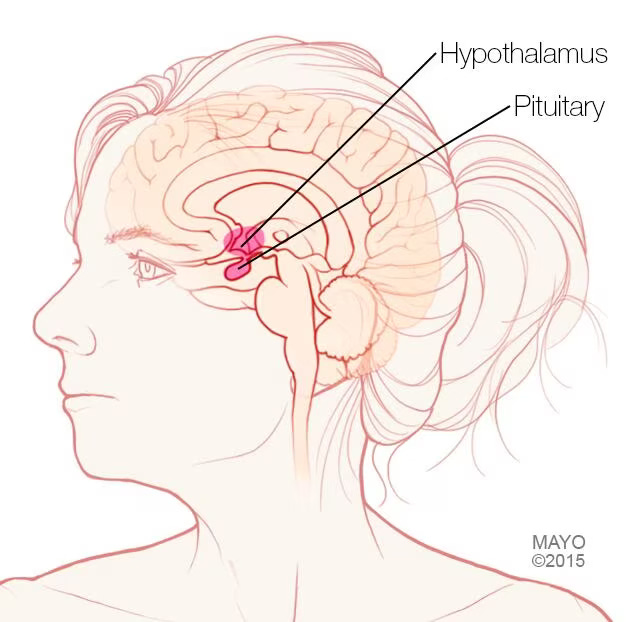
In addition to his multiple psychiatric comorbidities, Gary, who was taking testosterone, had what’s known as a prolactinoma. This is a benign tumor in the pituitary gland that drives excessive production of prolactin, a hormone that triggers breast milk production. This, Dr. Hamann said, “was extremely dysphoria-producing for Gary.” But Gary did not experience breast milk production spontaneously, she said. It began after he started testosterone and only occurred when he bound his breasts—which he did “very tightly,” according to Dr. Hamann.
Gary’s prolactin level was elevated. To determine the cause, Dr. Hamann teamed with his psychiatrist to take him off a low-dose of Abilify, which is an atypical antipsychotic, for a few weeks. The prolactin level then decreased but remained elevated. And yet Gary did not have all the typical symptoms of elevated prolactin, including headaches and visual changes; he just had the breast milk production.
Once Gary had top surgery—a double mastectomy—the breast milk problem was eliminated. So despite the persistent presence of the pituitary lesion, Dr. Hamann felt that no changes in Gary’s treatment were necessary at this time. The team could simply monitor him over time with routine MRIs and prolactin level testing.
“Now, as an endocrineology provider, does anybody like to hear you've got a six- or seven-millimeter pituitary lesion that we’re just going to not do anything about?” she said. “When we know we have a tool that has the potential to shrink the size of the prolactinoma? No, not really. But this is an idea, again, of what are our patient’s individual goals? What are we helping them to achieve?”
“I’ve seen in a variety of other situations where anyone that’s had any sexual abuse in their history, they are questioned if the sexual abuse caused the gender dysphoria. That’s not been my experience at all, certainly not with this individual, but in other situations as well.”
In discussing how antipsychotics impact dopamine, which in turn can affect prolactin, Dr. Schnitzlein addressed the tangled interplay between gender dysphoria and other psychiatric problems. She suggested that in some cases, affectations of gender dysphoria “can be written off as sometimes bipolar disorder, psychiatric disorders, associative disorders, anxiety disorders, because somebody’s uncomfortable in their own skin.” She then re-emphasized the importance of focusing on trauma.
Dr. Fenwick was eager to dispel what he suggested was a prevailing myth: that sexual trauma can drive gender dysphoria and transgender identification. “I’ve seen in a variety of other situations where anyone that’s had any sexual abuse in their history, they are questioned if the sexual abuse caused the gender dysphoria,” he said. “That’s not been my experience at all, certainly not with this individual, but in other situations as well.”
In Conclusion
Dr. Hamann said that her role was not to simply hand people hormones, but to take a thorough history and, while maintaining an open mind, to “figure out what other pieces might be going on so that we provide them with the safest, most informed endocrine care.”
“My one key takeaway,” Dr. Schnitzlein said, “is go into these encounters with an open mind and don’t make assumptions. Everyone’s journey is different, and our patients will, nine times out of 10, tell us what their needs are and what they’re hoping for.”
She concluded: “Don’t assume and don’t railroad.”
The WPATH Files: Report Derides Influential Trans-Medicine Group As ‘Unethical’
A damning new report based on a trove of leaked internal communications from the World Professional Association for Transgender Health has lambasted WPATH as “neither scientific nor advocating for ethical medical care.”
I am an independent journalist, specializing in science and health care coverage. I contribute to The New York Times, The Guardian, NBC News and The New York Sun. I have also written for the Washington Post, The Atlantic and The Nation. Follow me on Twitter: @benryanwriter and Bluesky: @benryanwriter.bsky.social. Visit my website: benryan.net








Great work as always, Benjamin!
It's amazing hearing doctors say they have an opinion about a patient but they wouldn't want their judgment to take precedence over the expertise of the patient. A patient who is explicitly seeking help from a doctor. What must these doctors think the point of a doctor is? Just being a pathway to drugs and treatment? I struggle to fathom how this makes sense in any other context in medicine. "When a patient says they want Oxycontin, don't railroad them! Just meet them where they are on their journey of pain relief!"
I've listened to quite a few WPATH presentations at this point (I think it's good to know how they speak with each other on these topics). It's actually pretty unusual to come across a really bonkers, quotable moment, and on the surface no one comes off like a villain. What you get is a bunch of well-intentioned people who live in a shared reality where the following things are true (repurposed from a comment I made on a different post earlier this year): 1) everyone has an innate, ineffable, but also potentially flexible thing called a "gender identity", 2) for people whose bodies don’t align with their gender identity, the greatest and highest good is to alter their body with hormones and surgeries to bring the two into alignment, 3) these are safe, effective, and ALWAYS medically necessary, 4) anything interfering with easy access to these is “gatekeeping” and is bad, 5) anything that normalizes them and makes them easier to get is “gender affirming” and is good, 6) the gender affirming community is a small, brave, beleaguered community defending access to these treatments against dark forces who are conspiring to take them away.
And that's how you end up with earnest conversations like this. None of these individuals should have even come close to getting (or nearly getting) these procedures but for the ideology motivating the doctors. Worse, the ideology actively interferes with the patient getting treatments that are more likely to help them in the long term and are much less invasive, like learning distress tolerance and resilience, CBT, ACT, and even psychiatric medications when necessary. And when they do, like in the case of the patient who was prescribed the SSRI, it seems to be in spite of the ideology or as a stopgap until they can get the "real" treatment of sex-trait modification procedures.
It's its own kind of tragedy. These are doctors who clearly mean well and want to do good, but for various social reasons have been taken in by an ideology that has hijacked those good intentions to actively do medical harm to the very people they want to help.