How Gordon Guyatt's 'Values and Preferences' Triggered His Fall From Grace
The "godfather of evidence-based medicine" shocked and appalled skeptics of pediatric gender medicine by adopting activist rhetoric last month that contradicted his own team's research.

This Substack serves as an addendum to the article I published Tuesday in
, which I encourage you to check out. In that investigative effort, I plumb the depths of the sprawling scandal concerning Dr. Gordon Guyatt, one of the so-called “godfathers of evidence-based medicine.” Dr. Guyatt shocked and appalled skeptics of pediatric gender medicine on Aug. 14 when he and four of his colleagues at McMaster University in Canada published a statement in which they caved to transgender-activist pressure and took sides in the political debate over the U.S. bans on puberty blockers and cross-sex hormones for minors.Earlier this year, the Guyatt team published a trio of systematic literature reviews that found that gender-transition treatments and mastectomies for youths were all based on weak and uncertain evidence. In their recent statement, the five McMaster experts who signed it condemned the use of their research to support bans of such interventions. And importantly, they contradicted their own research findings by using activist (and unscientific) rhetoric like “medically necessary” and “hormone replacement therapy” to characterize these treatments.
In this Substack, I will:
Go into greater depth about the ethical debates between Dr. Guyatt and others behind the effort to develop evidence-based treatment guidelines for pediatric gender medicine.
Publish detailed statements from Dr. Guyatt that he made at the Society for Evidence Based Gender Medicine (SEGM) conference in New York in October 2023, which I attended. These remarks will help clarify his point of view on how evidence-based-medicine principles should guide pediatric gender medicine clinical decision-making. The quotes will also indicate at least one way that Dr. Guyatt contradicted himself in his Aug. 14 statement.
Call into question Dr. Guyatt’s recent astonishing claim to
that he didn’t know until a few months ago that since 2021, SEGM was funding his team’s work on the gender-medicine review papers. In their August statement, Dr. Guyatt and his colleagues disavowed SEGM in oblique terms, suggesting that the nonprofit is not truly grounded in science, but failing to explain their reasoning.Publish internal emails that I obtained of the McMaster team deliberating over how to respond to mounting activist pressure for them to distance themselves from the “misuse” of their work by those seeking to cause “harm”.
The Great Values & Preferences Debate
At the core of the debate that has blown up in Dr. Guyatt’s face is a tension between him and SEGM over the relative importance, in evidence-based medical guidelines and clinical decision-making, of what are known as values and preferences. In the statement Dr. Guyatt’s team published in August, they said that “a high respect for autonomy” of patients “becomes particularly important when the certainty of the evidence is low or very low,” as is the case in pediatric gender medicine. They continued: “In such circumstances, clinicians should work with patients to ensure that care reflects the experience, goals, and priorities of those needing care—that is, their values and preferences.”
Moti Gorin, a philosopher and bioethicist at Colorado State University, told me he was troubled by this suggestion, which he and other experts I spoke with said reduced pediatric gender medicine to barely more than a consumer economy—and one servicing vulnerable youths who often have considerable mental health problems at that. These experts argued that while the evidence may also generally be weak supporting the potential harms of gender-transition interventions to minors, those harms, including fertility loss, are considerable. They also said Dr. Guyatt was stepping out of his lane and addressing broader questions of how his work should be interpreted that are properly left to ethicists, legal experts and policy makers.
In particular, these experts argued that Dr. Guyatt had a clear habit of over-emphasizing the importance of patient autonomy and failing to properly take into consideration the three other pillars of evidence-based clinical decision-making:
beneficence (the physician’s imperative to help the patient)
non-maleficence (the physician’s imperative not to harm the patient)
justice ( fair access to resources, equitable access to care)
Some of the experts I spoke with told me they were alarmed that Dr. Guyatt seemed to be cavalier with respect to doctors’ responsibility to protect patients from themselves.
“Physicians have a duty not to harm,” said Mikael Landén, a principal researcher at the Karolinska Institutet in Stockholm and coauthor of Sweden’s systematic review of pediatric gender medicine. “If a physician judges that a treatment carries significant risks with little chance of benefit, it is unethical to prescribe it—even if the patient requests it.”
Sweden, he said, had struck a “reasonable balance” by restricting pediatric access to gender-transition drugs to carefully considered “exceptional cases” only in research settings.
Rachel Couban, the McMaster librarian on the SEGM-commissioned reviews, objected in an email to the premise that Dr. Guyatt’s reputation was threatened by the group’s August statement, which she signed. “Dr. Guyatt has dedicated his life to promoting fair and equitable access to treatment, and he pretty well invented the concept of quality of life research,” she said. “Quality of life is an important concept for this gender situation. We all want the best for our kids.”
During SEGM’s 2023 meeting in New York, there was a lively panel discussion with Dr. Guyatt, Dr. Gorin and others about the relative importance of patient values and preferences. Some of the panelists who challenged Dr. Guyatt for placing such an emphasis on these factors argued that if a youth with gender dysphoria is misinformed about the promise of gender-transition by adults who inflate its benefits, then this subverts the informed consent process; and it calls into question whether the youth’s values and preferences can truly be trusted as a compass for clinical decision-making.
“Clinicians never have and never should have the obligation to give interventions that they think are not in the patient’s best interest.” —Dr. Gordon Guyatt
On the panel, Dr. Guyatt acknowledged: “Clinicians never have and never should have the obligation to give interventions that they think are not in the patient’s best interest.” He continued: “I would say your obligation is to make it clear to the patient that you think they are misguided and that their current plan and course of action is actually not in their best interest.”
Prior to the panel discussion, Dr. Guyatt gave a lecture outlining the basics of evidence-based medicine, including the widely used GRADE system he devised earlier in his career to analyze medical research (and which his team employed for their SEGM-commissioned reviews). He was adamant and transparent about being a neophyte on the topic of pediatric gender medicine. “I’m a specialist in hospital-based internal medicine,” he said. “I have nothing to do with pediatrics, and I’ve had nothing to do clinically with gender medicine.” He apologized in advance for any misinformed statements he might make on the subject.
A conference presentation given before Dr. Guyatt’s talk had suggested that in Finland, youths who presented to gender clinics with a high level of psychiatric comorbidities did not tend to improve on gender-transition drugs. Consequently, Dr. Guyatt opined during his own lecture that these medications would be unlikely to help this profile of patient (which happens to be the typical profile of youths presenting at gender clinics these days). He then suggested that it would be nice if there were some sort of test to determine who would do well on such drugs and who would not. (Leaders in the pediatric gender medicine field have never sought to establish any such test—especially not now, with so many of the American leaders, such as. Dr. Johanna Olson-Kennedy, denouncing psychological assessments in advance of starting kids on puberty blockers as harmful “gatekeeping.”)
On the subsequent panel, Dr. Guyatt argued that while very young children likely cannot participate fully in the informed consent process, eventually, as a child goes through adolescence, there needs to be a point at which adults begin to consider that young person as medically autonomous and able to fully weigh in on their own care.
“Most of us would agree that you’re going to put less value in the children’s autonomy when they’re nine,” Dr. Guyatt said, “and you might put more when they’re 14, and you’ll certainly put more when they’re 18. Where is the threshold where you start the value of child autonomy?”
He later continued: “Once you decide that the child is old enough to participate in the discussion with the participation of their parents, then you are in a situation of full, appropriate, informed decision-making that considers people’s values and preferences.”
“The evidence alone is never enough,” Dr. Guyatt also said, “and the decision process, especially when the evidence is very low quality, which means we’re not certain actually [then] the weight of the decision essentially shifts to the patient’s values and preferences. At the very least, patient values and preferences should play a key role, depending on how one interprets those treatments.”
Others on the panel, as well as experts I spoke with more recently, are more inclined to believe that because the diagnosis of gender dysphoria is so subjective and its stability is so uncertain, this calls into question whether doctors can really put so much faith into a gender-distressed minor patient’s wants and needs if that young person seeks blockers and hormones. This holds especially true given the potential major irreversible impacts of this treatment pathway and sets these treatments apart from, say, standard psych meds for youths, these experts said.
On the panel, Dr. William Malone, an endocrinologist in Twin Falls, Idaho, and SEGM’s cofounder, spoke to what he characterized as the considerable potential harms of pediatric gender-transition treatment. “A 12 year old cannot consent to a lifetime of infertility and sexual dysfunction,” he said. (Note that a recent study called into question longstanding claims that these drugs cause particularly severe sexual dysfunction when begun during adolescence. But more research is needed.) “So I don’t even understand how to begin to approach a values-and-preferences conversation with someone that young about things they've never experienced.”
Referring to a theoretical figure, Dr. Malone said that we would “have to know these interventions are going to save this number of lives over this period of time. That perhaps would justify a certain number of sterilized individuals who would have severe, crushing regret later in life. We don’t have any of that information. So I don’t understand how these interventions are being offered so indiscriminately in the United States. Currently, I’m heartened to see the rollback in Europe, that seems to be the logical conclusion when you have uncertainty of evidence and certainty of harm.”
When Did Dr. Guyatt Learn SEGM Sponsored His Team’s Research?
In his recent bombshell interview with Jesse Singal, Dr. Guyatt strained credulity among many stakeholders when he claimed that he was unaware until a few months ago that SEGM was funding his team’s reviews. The contract with SEGM, after all, began in 2021 and was extended in 2024. Plus, Dr. Guyatt attended the SEGM conference in the fall of 2023 (albeit, only for a portion of one of the two-and-a-half days of the gathering), which also saw a few of his colleagues give presentations.
Dr. Romina Brignardello-Peterson is an associate professor of health-research methods at McMaster University and led the team under Dr. Guyatt that, per SEGM’s commission, conducted the five systematic reviews of the evidence behind various gender-transition interventions for youths. Dr. Guyatt was present at the SEGM conference the day that Dr. Brignardello-Peterson gave a presentation in which she previewed the findings of the McMaster review on mastectomies for people under age 26.
At the opening of her presentation, Dr. Brignardello-Peterson stated: “I’ve been a consultant for SEGM for about two and a half years.” And then she said that the mastectomy review was “part of a research agreement between SEGM and McMaster University,” displaying a slide that said as much.
SEGM, Dr. Brignardello-Peterson said, defined the question of interest for the review. The funds, she said, supported the three graduate students working on the project, plus a small salary for her.
It remains possible that Dr. Guyatt was out of the room at the time of Dr. Brignardello-Peterson’s presentation; I have been unable to find any documentation indicating whether he was indeed in the room at that time.
The McMaster Emails
Dr. Steven Montmante, an independent plastic surgeon in Richmond, Virginia, who performs gender-transition surgeries (but on adults only), was a coauthor on four of the McMaster reviews about pediatric gender medicine. This includes one pending paper on so-called “binding” and “tucking” among youth that the McMaster team has sought to divorce themselves from before publication. He provided me emails that Dr. Brignardello-Peterson earlier this year sent to him and the other coauthors on her and Dr. Guyatt’s behalf. In the emails, the pair made suggestions about how to go public with the assertion that they were unhappy that their review papers were being “misused and may be causing harm.”
“[O]ur work is being misused and may be causing harm.” —Dr. Romina Brignardello-Peterson
In the first email, the two McMaster professors suggested that they add a new paragraph to the conclusion of their papers, three of which had already been published, emphasizing the importance of patient autonomy.
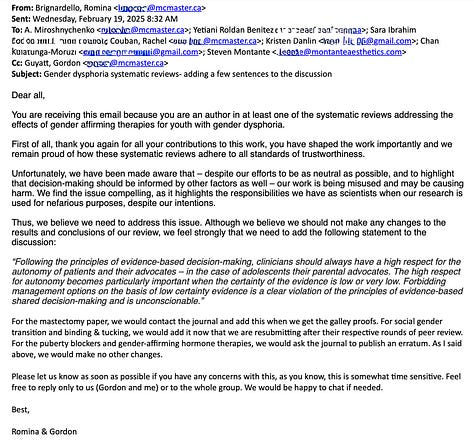
Feb. 19, 2025:
Dear all,
You are receiving this email because you are an author in at least one of the systematic reviews addressing the effects of gender affirming therapies for youth with gender dysphoria.
First of all, thank you again for all your contributions to this work, you have shaped the work importantly and we remain proud of how these systematic reviews adhere to all standards of trustworthiness.
Unfortunately, we have been made aware that – despite our efforts to be as neutral as possible, and to highlight that decision-making should be informed by other factors as well – our work is being misused and may be causing harm. We find the issue compelling, as it highlights the responsibilities we have as scientists when our research is used for nefarious purposes, despite our intentions.
Thus, we believe we need to address this issue. Although we believe we should not make any changes to the results and conclusions of our review, we feel strongly that we need to add the following statement to the discussion:
“Following the principles of evidence-based decision-making, clinicians should always have a high respect for the autonomy of patients and their advocates – in the case of adolescents their parental advocates. The high respect for autonomy becomes particularly important when the certainty of the evidence is low or very low. Forbidding management options on the basis of low certainty evidence is a clear violation of the principles of evidence-based shared decision-making and is unconscionable.”
For the mastectomy paper, we would contact the journal and add this when we get the galley proofs. For social gender transition and binding & tucking, we would add it now that we are resubmitting after their respective rounds of peer review. For the puberty blockers and gender-affirming hormone therapies, we would ask the journal to publish an erratum. As I said above, we would make no other changes.
Please let us know as soon as possible if you have any concerns with this, as you know, this is somewhat time sensitive. Feel free to reply only to us (Gordon and me) or to the whole group. We would be happy to chat if needed.
Best,
Romina & Gordon
In response, Dr. Montante expressed his misgivings about such a plan and the off-target effects it could have. He responded to all his fellow review coauthors.
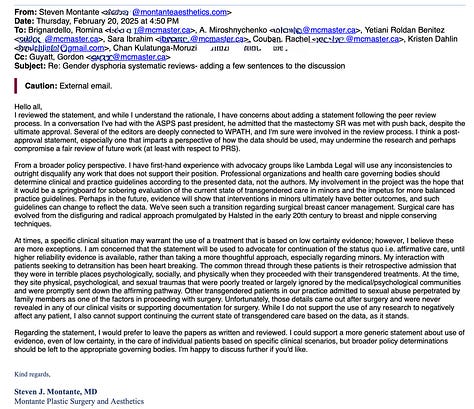
Feb. 20, 2025
Hello all,
I reviewed the statement, and while I understand the rationale, I have concerns about adding a statement following the peer review process. In a conversation I've had with the ASPS past president, he admitted that the mastectomy SR was met with push back, despite the ultimate approval. Several of the editors are deeply connected to WPATH, and I'm sure were involved in the review process. I think a post-approval statement, especially one that imparts a perspective of how the data should be used, may undermine the research and perhaps compromise a fair review of future work (at least with respect to PRS).
From a broader policy perspective. I have first-hand experience with advocacy groups like Lambda Legal will use any inconsistencies to outright disqualify any work that does not support their position. Professional organizations and health care governing bodies should determine clinical and practice guidelines according to the presented data, not the authors. My involvement in the project was the hope that it would be a springboard for sobering evaluation of the current state of transgendered care in minors and the impetus for more balanced practice guidelines. Perhaps in the future, evidence will show that interventions in minors ultimately have better outcomes, and such guidelines can change to reflect the data. We've seen such a transition regarding surgical breast cancer management. Surgical care has evolved from the disfiguring and radical approach promulgated by Halsted in the early 20th century to breast and nipple conserving techniques.
At times, a specific clinical situation may warrant the use of a treatment that is based on low certainty evidence; however, I believe these are more exceptions. I am concerned that the statement will be used to advocate for continuation of the status quo i.e. affirmative care, until higher reliability evidence is available, rather than taking a more thoughtful approach, especially regarding minors. My interaction with patients seeking to detransition has been heart breaking. The common thread through these patients is their retrospective admission that they were in terrible places psychologically, socially, and physically when they proceeded with their transgendered treatments. At the time, they site physical, psychological, and sexual traumas that were poorly treated or largely ignored by the medical/psychological communities and were promptly sent down the affirming pathway. Other transgendered patients in our practice admitted to sexual abuse perpetrated by family members as one of the factors in proceeding with surgery. Unfortunately, those details came out after surgery and were never revealed in any of our clinical visits or supporting documentation for surgery. While I do not support the use of any research to negatively affect any patient, I also cannot support continuing the current state of transgendered care based on the data, as it stands.
Regarding the statement, I would prefer to leave the papers as written and reviewed. I could support a more generic statement about use of evidence, even of low certainty, in the care of individual patients based on specific clinical scenarios, but broader policy determinations should be left to the appropriate governing bodies. I'm happy to discuss further if you'd like.
Kind regards,
Steven J. Montante, MD
Montante Plastic Surgery and Aesthetics
Dr. Brignardello-Peterson and Dr. Guyatt then backpedaled. They scrapped the idea of adding the new paragraph to the papers’ conclusions. Instead, they ultimately proposed sending a letter to the editors of all the journals that had published or would publish their reviews on gender medicine, detailing their concerns that their work was being misused, ostensibly to cause harm.
First, the pair emailed the coauthors the following:
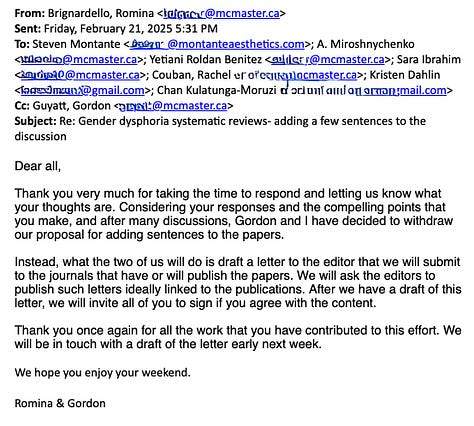
Feb. 21, 2025
Dear all,
Thank you very much for taking the time to respond and letting us know what your thoughts are. Considering your responses and the compelling points that you make, and after many discussions, Gordon and I have decided to withdraw our proposal for adding sentences to the papers.
Instead, what the two of us will do is draft a letter to the editor that we will submit to the journals that have or will publish the papers. We will ask the editors to publish such letters ideally linked to the publications. After we have a draft of this letter, we will invite all of you to sign if you agree with the content.
Thank you once again for all the work that you have contributed to this effort. We will be in touch with a draft of the letter early next week.
We hope you enjoy your weekend.
Romina & Gordon
A month later, they also wrote:
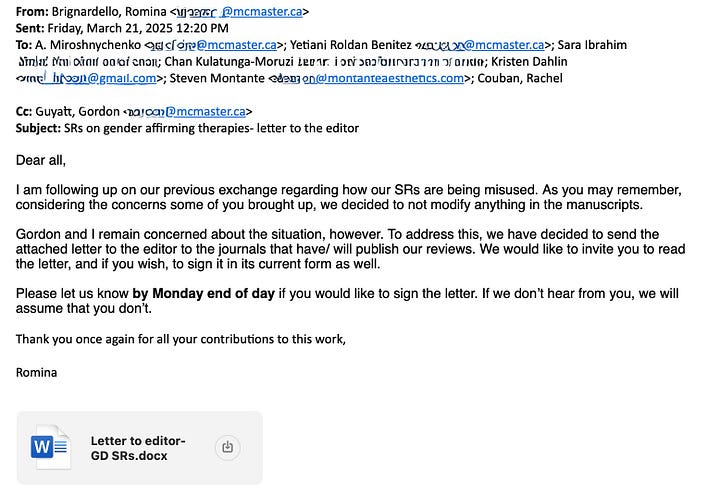
March 21, 2025
Dear all,
I am following up on our previous exchange regarding how our SRs are being misused. As you may remember, considering the concerns some of you brought up, we decided to not modify anything in the manuscripts.
Gordon and I remain concerned about the situation, however. To address this, we have decided to send the attached letter to the editor to the journals that have/ will publish our reviews. We would like to invite you to read the letter, and if you wish, to sign it in its current form as well.
Please let us know by Monday end of day if you would like to sign the letter. If we don’t hear from you, we will assume that you don’t.
Thank you once again for all your contributions to this work,
Romina
Here is the draft of the letter to the editor that was included as a Word document attachment to the March 21 email. It is very similar to the statement that five members of the McMaster team ultimately published on the university website in August.
Dear Editor,
Authors of scientific articles have a responsibility to attend to how their contributions will be used and to modify their presentation in the articles, or other communication, accordingly. We, X of the authors of (info to identify article) are concerned that the conclusions of our work, that only low certainty evidence exists (as determined by the Grading of Recommendations Assessment, Development, and Evaluation approach) regarding the benefits of the gender-affirming care interventions addressed in our review, will be misused. Specifically, we are concerned our findings will be used to justify denying medical care (such as puberty blockers and hormone replacement therapy) to trans, nonbinary, and gender-diverse (TGD) individuals. Indeed, our prior work has been used in exactly this highly problematic way.
We therefore feel compelled to make explicit our view regarding how our findings should and should not be used. Following fundamental principles of humane medical practice, clinicians have an obligation to care for and with those in need. It is unconscionable to forbid clinicians from delivering gender-affirming care.
Moreover, following the principles of evidence-based decision-making, clinicians should always have a high respect for the autonomy of patients and their advocates. The high respect for autonomy becomes particularly important when the certainty of the evidence is low or very low. In these cases, the reasons to treat and how to do so must draw mostly from the experience, goals, and priorities of those needing care.
It is disingenuous to cast health care based on low-certainty evidence as bad care or as care driven by ideology, and low-certainty evidence as bad science. Furthermore, forbidding delivery of gender-affirming care and limiting medical management options on the basis of low certainty evidence is a clear violation of the principles of evidence-based shared decision-making and is unconscionable. The appropriate use of our work is in ensuring patients receive needed care and in helping TGD patients and their clinicians in decision making.
We write this statement in the hope that all those who use our work to inform the care of TGD patients receiving gender-affirming care, and those using our work in consideration of policy decisions, continue to centre the autonomy of the TGD patient.
Gordon H Guyatt
Romina Brignardello-Petersen
Dr. Montante told me that he declined to sign the letter to the editor. After that, Drs. Bignardello-Peterson and Guyatt did not ask him to sign the statement published in August, and in fact never broached the subject of the statement to him before they published it. He told me he figured that whoever had declined to sign the letter to the letter was then left out of the loop about the statement, which four of the nine coauthors, including him, did not sign.
Note that Dr. Montmante and I spoke at length last week. I will be publishing a detailed Q&A of our conversation at some point over the next few days. So stay tuned and subscribe if you haven’t already.
I am an independent journalist, specializing in science and health care coverage. I contribute to The New York Times, The Guardian, NBC Newsand The New York Sun. I have also written for the Washington Post, The Atlantic and The Nation. Follow me on Twitter: @benryanwriter and Bluesky: @benryanwriter.bsky.social. Visit my website: benryan.net








These were excellent articles, the Unherd one and this one. You mention that Dr. Guyatt has been accused of having a history of overemphasizing patient autonomy. Do you know if these any of these other instances were also heavily political or activist influenced? For example, would he have responded to the Marcolino et al 2022 systematic review that did not find good evidence for using ivermectin to treat Covid infections as a way to reduce mortality or ventilator use by also saying this should result in more patient autonomy in getting ivermectin if they wanted it, especially for their children? In other words, is there evidence that Dr. Guyatt consistently responds this way to all SRs with weak outcomes, or are only certain ones - high profile, politicized, or highly activist influenced - getting this response?
The Atlantic just published a big article about medically assisted death in Canada that touches on many of the same ethical debates. It says, "When autonomy is entrenched as the guiding principle, exclusions and safeguards eventually begin to seam arbitrary and even cruel."
The article contrasts euthanasia in Canada to Europe, where there are more legal limitations on who is eligible. It seems our North American culture has a big impact on medical ethics. Without clear legal guidelines, that field of medicine selects for extremists doctors who support the procedure even in edge cases.
Here is a quote from one of the MAiD doctors: “Once you accept that people ought to have autonomy—once you accept that life is not sacred and something that can only be taken by God, a being I don’t believe in—then, if you’re in that work, some of us have to go forward and say, ‘We’ll do it.’ ”